After-hour ICU Discharges
By Yisrael M Safeek, MD, MBA, CPE, FACPE
By Yisrael M Safeek, MD, MBA, CPE, FACPE
USA
August 12, 2015
August 12, 2015
A review of the literature has consistently shown that after-hours ICU discharges contributes to adverse care events, including preventable hospital deaths.
A review of the literature has consistently shown that after-hours ICU discharges contributes to adverse care events, including preventable hospital deaths. After-hours discharges are those between 6 p.m.-6 a.m. After-hour ICU discharges is a national quality of care indicator in Australia, New Zeeland, and the United Kingdom. The largest study of its kind involved Australian and New Zealand Intensive Care Society Adult Patient Database prospectively records data on patients in 90% of Australian and 50% of New Zealand ICUs. The results of this large retrospective registry study was published in the October issue of Intensive Care Medicine.
Between January 2005 and December 2012, researchers examined whether discharge from the ICU to the general ward after regular hours were associated with increased in-hospital mortality and ICU readmission. The analysis included 710,535 patients discharged alive from the ICU, of which 109,384 (15.4 %) were discharged after-hours. Patients discharged after-hours had a higher hospital mortality (6.4% versus 3.6 %) and more ICU readmissions (5.1% versus 4.5 %) than patients discharged during regular hours. Although post-ICU mortality declined during the study period, the risk associated with after-hours discharge remained elevated throughout.
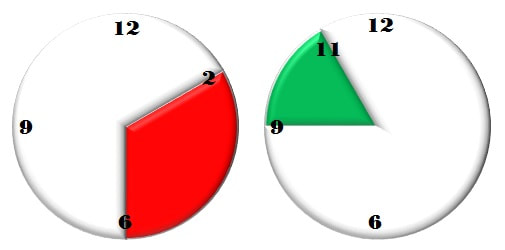
When the data were examined according to the actual hour of ICU discharge, the highest mortality risk occurred with those who left between 2a.m.-6 a.m. and the lowest between 9 a.m.-11 a.m. (Figure 1). Patients who left the ICU between 6 p.m.-6 a.m. were also significantly more likely to be readmitted to the unit during their hospital stay (5.1% vs. 4.5%). While comparable data from the United States are not readily available, there is little reason to assume that the situation is different here.
Between January 2005 and December 2012, researchers examined whether discharge from the ICU to the general ward after regular hours were associated with increased in-hospital mortality and ICU readmission. The analysis included 710,535 patients discharged alive from the ICU, of which 109,384 (15.4 %) were discharged after-hours. Patients discharged after-hours had a higher hospital mortality (6.4% versus 3.6 %) and more ICU readmissions (5.1% versus 4.5 %) than patients discharged during regular hours. Although post-ICU mortality declined during the study period, the risk associated with after-hours discharge remained elevated throughout.
When the data were examined according to the actual hour of ICU discharge, the highest mortality risk occurred with those who left between 2a.m.-6 a.m. and the lowest between 9 a.m.-11 a.m. (Figure 1). Patients who left the ICU between 6 p.m.-6 a.m. were also significantly more likely to be readmitted to the unit during their hospital stay (5.1% vs. 4.5%). While comparable data from the United States are not readily available, there is little reason to assume that the situation is different here.
Figure 1. AM time periods for worst and best mortality rates after ICU Discharges.
Previous observational studies had described an association of after-hours discharges from the ICU with higher hospital mortality and readmission rates in Australia, New Zealand, the United Kingdom, Canada and France. A 2015 English study with retrospective data for patients admitted to the ICU from April 2007 to September 2014 again documented this association between critical care discharge time and hospital mortality, to a statistically significant level. There were 2,711 patients discharged during daytime hours, of which 145 (5.35%) died. A total of 478 patients were discharged at night, of which 40 died (8.37%). ICU readmission rate was 5.2% by day, and 6.1% at night.
Why should after-hours discharges from the ICU be a contributor to preventable hospital deaths and what are contributing factors? First, busy ICUs tend to “overflow” and transfer out “lesser sick” patients. Second, in ICUs lacking 24/7 intensivists, the decision to transfer may be made by less experienced clinicians. Third, patient handoffs may also be less complete after hours due to staffing levels on the wards that are lower than in the ICU.
Regardless of the reasons of preventable hospital deaths from after-hours ICU discharges, there are still lingering questions. Should all after-hour discharges be audited? Should a standard assessment tool for ICU discharge readiness be developed? Should specific quality standards around after-hours ICU discharges be necessitated?
Why should after-hours discharges from the ICU be a contributor to preventable hospital deaths and what are contributing factors? First, busy ICUs tend to “overflow” and transfer out “lesser sick” patients. Second, in ICUs lacking 24/7 intensivists, the decision to transfer may be made by less experienced clinicians. Third, patient handoffs may also be less complete after hours due to staffing levels on the wards that are lower than in the ICU.
Regardless of the reasons of preventable hospital deaths from after-hours ICU discharges, there are still lingering questions. Should all after-hour discharges be audited? Should a standard assessment tool for ICU discharge readiness be developed? Should specific quality standards around after-hours ICU discharges be necessitated?
Unless otherwise noted, you can republish our articles for free under a Creative Commons license. Here’s what you need to know:
- You have to credit us. In the byline, we prefer “Author Name, SafeCare.” At the top of the text of your story, include a line that reads: “This story was originally published by SafeCare magazine.” You must link the word “SafeCare" to the original URL of the story https://www.safecaremagazine.com/safecare-afterhour-discharges.html